Diabetic retinopathy is one of the leading causes of blindness in the United States. All diabetics should have a thorough dilated eye exam every year to detect the presence of diabetic retinopathy.
What are the Symptoms of Diabetic Retinopathy?
Blurry vision and floaters may be symptoms of diabetic retinopathy, but many patients may not have any symptoms.

How Does Diabetes Affect the Eye?
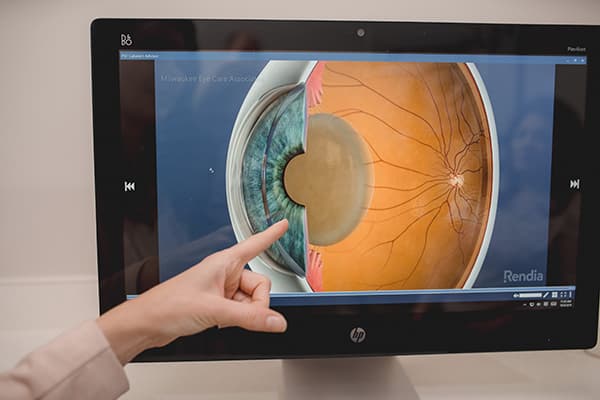
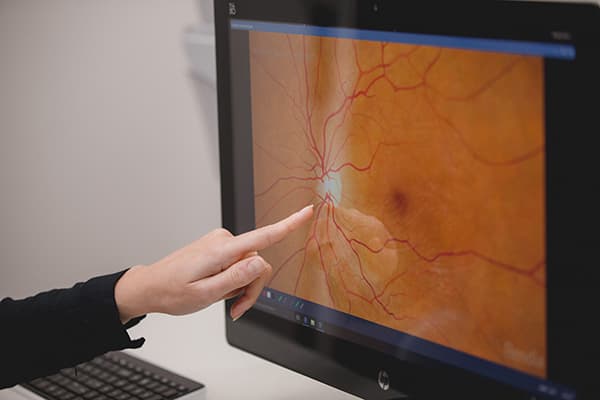
High blood sugars from diabetes can damage the small blood vessels in the retina (the nerve tissue that lines the eye). As a result, the blood vessels begin to bleed and leak and the retina does not receive enough oxygen. This is termed “diabetic retinopathy.” When the leaking of blood vessels causes retinal swelling and decrease in vision, this is called “diabetic macular edema.”
Types of Diabetic Retinopathy:
Background or Non-proliferative retinopathy:This type of retinopathy is characterized by small areas of bleeding and weak spots in the blood vessels called micro-aneurysms.
Proliferative retinopathy:A more advanced form of diabetic retinopathy where the retina is not receiving adequate oxygen and new blood vessels begin to grow, called “neovascularization.” Unfortunately, these vessels are abnormal and can cause many problems, including loss of vision due to bleeding, glaucoma, and retinal detachment.
Diabetic Macular Edema: Swelling of the retina due to leaky blood vessels and often causes a decrease in central vision.
What are the Risk Factors for Diabetic Retinopathy?
Elevated blood sugar over time, duration of diabetes, high blood pressure, sleep apnea, high cholesterol, and pregnancy.
What is the Treatment of Diabetic Retinopathy?
Mild diabetic retinopathy may be routinely monitored by your eye doctor, but a retina specialist may be involved for treatments including injections, laser, or surgery.

- Prevention: The best treatment is prevention. Many cases can be prevented or controlled by adequate control of blood sugar, blood pressure, and cholesterol.
- Anti-VEGF Injections: In some cases, a medication may be injected into the eye to help control diabetic macular edema or retinopathy. Medications commonly used are “anti-VEGF” or steroids. Anti-VEGF medications target the VEGF molecule, which is believed to drive the process of neovascularization and swelling in the retina. Commonly used anti-VEGF medications are Avastin, Eylea, or Lucentis. Commonly used steroids are Triessence or Ozurdex.
- Laser: Laser, which is a therapy using light beams, may be used to treat leaky blood vessels in diabetic macular edema or abnormal new blood vessels in proliferative diabetic retinopathy.
- Surgery: Surgery is reserved for advanced cases of diabetic retinopathy where vision is threatened by prolonged bleeding or retinal detachments. These surgeries are performed by retina surgeons.