One of the most commonly expressed concerns from patients is the fear of developing age-related macular degeneration. This concern is justified, as age-related macular degeneration (AMD) is the leading cause of permanent vision loss in people 60 years of age or older. The exact cause of AMD isn’t known, although it’s more common in people with a family history. It’s also more common in Caucasians, females, and smokers, although age is the greatest risk factor.
What is AMD?
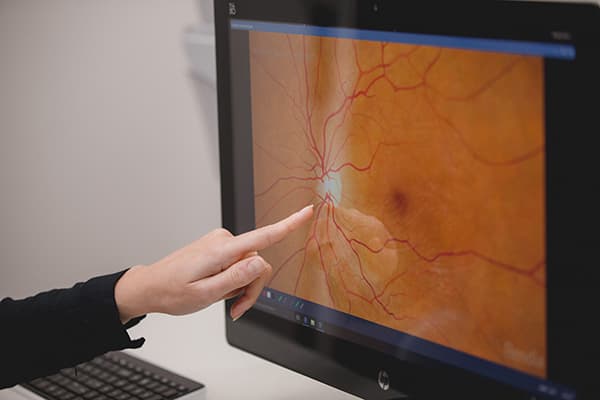
AMD is degeneration of the small, specialized part of the retina called the macula, which provides us with our fine focus and detail vision. It is the central part of the retina that is responsible for central vision used in reading or seeing details. It is a slowly progressive condition, but may be so mild that vision loss isn’t noticed. Although peripheral (side) vision is valuable in mobility and in providing awareness of the environment, peripheral vision gives only about 20/200 resolution. In contrast, the macula in a normal healthy eye generally has 20/20 vision (with glasses, if needed). This means that the macula is ten times better at resolving detail than the peripheral retina.
Early symptoms include trouble seeing small print, blurriness, or distortion in the center of vision. In some people, central vision loss may deteriorate quickly and require treatment to stabilize or prevent further vision loss.
It is important to understand that AMD, by itself, does not lead to total blindness, as the peripheral vision is left intact. The term “legal blindness” is used to describe vision which cannot be improved to better than 20/200 with glasses or contact lenses, and is a definition used to determine eligibility for social services.

What is the difference between Wet and Dry AMD?
Dry AMD
Dry AMD is the most common form of macular degeneration. During its earliest stages, yellow, crystal-like deposits called drusen form in the retina. These drusen consist of waste products that the retinal cells cannot break down. In some cases, dry AMD may progress to severe central vision loss.
Wet AMD
Wet AMD is a less common but more aggressive form of macular degeneration. It involves the formation of abnormal and fragile blood vessels beneath the retina, leading to swelling and bleeding. Early detection of wet AMD allows for the use of medications directly injected into the eye to shrink these abnormal vessels, minimizing further vision loss.
Treatment Options for AMD
 Studies have proven that patients with moderate to advanced Dry or Wet AMD are less likely to get worse if they take a combination of antioxidant vitamins and minerals known as the AREDS2 formula. AREDS stands for Age-Related Eye Disease Study. However, individuals with mild AMD or only a family history of the disease may benefit from a multivitamin instead.
Studies have proven that patients with moderate to advanced Dry or Wet AMD are less likely to get worse if they take a combination of antioxidant vitamins and minerals known as the AREDS2 formula. AREDS stands for Age-Related Eye Disease Study. However, individuals with mild AMD or only a family history of the disease may benefit from a multivitamin instead.
Wet AMD
For active bleeding and leaking in Wet AMD, treatment with anti-VEGF injections is indicated to stop the abnormal blood vessels and preserve vision. Commonly used anti-VEGF medications are Avastin, Eylea, or Lucentis.
Geographic Atrophy
What exactly is Geographic Atrophy?
Geographic Atrophy is a feature of advanced age-related macular degeneration, an eye condition that primarily affects the central portion of the retina, known as the macula. The macula is responsible for sharp, detailed vision, essential for tasks like reading, recognizing faces, and driving. Over time, macular degeneration caused the retinal cells in the macula to become sick and die. This leaves behind a blind spot which can slowly expand or grow over time and cause central vision loss. These areas are referred to as Geographic Atrophy.
What causes Geographic Atrophy?
Geographic Atrophy is a feature of advanced age-related macular degeneration (AMD), which is related to age, genetic factors, and lifetime exposure to smoking, UV damage, and other environmental factors. When retinal cells become sick from AMD, they can die and leave behind a blind spot. This process has been recently linked to the complement system of inflammation.
What are the symptoms of Geographic Atrophy?
The symptoms of Geographic Atrophy can vary from person to person, but the most common signs to look out for include blurry vision, blind spots, and difficulty seeing fine details. You may also notice distortions in straight lines or changes in color perception. As the disease progresses, these symptoms can significantly affect your ability to read, drive, or recognize faces.
What treatment options are available for Geographic Atrophy?
Up until recently, no treatment options were available for Geographic Atrophy. In 2023, the US Food and Drug Administration (FDA) approved a medication that was proven successful in slowing down the progression of geographic atrophy. The medication is a complement inhibitor, and blocks a series of chemical reactions believed to contribute to Geographic Atrophy progression. The medication is administered as an injection into your eye on a regular schedule. These treatments are now available at Milwaukee Eye Care with Dr. Mackenzie Sward.
Complement Inhibitor Injections
Intravitreal Injections have been around for many years for treatment of wet age-related macular degeneration, diabetic complications, and other diseases. Intravitreal injections are performed in our clinic on a regular schedule. Complement Inhibitors currently approved for the treatment of Geographic Atrophy include IZERVAY™ (Avacincaptad pegol) and SYFOVRE™ Pegcetacoplan).
What can I expect from Complement Inhibitor Treatment for GA?
The treatments are aimed at slowing the disease progression of Geographic Atrophy. The treatments unfortunately do not reverse existing retinal damage from AMD or improve the vision. The treatments also do not prevent any further vision loss from occurring. This means that these treatments might help protect your central vision for a longer period.
As with all treatments, there are risks. Not everyone with age-related macular degeneration is a candidate for these treatments. It is best to review these risks and considerations with your doctor.
Other Recommendations for AMD:
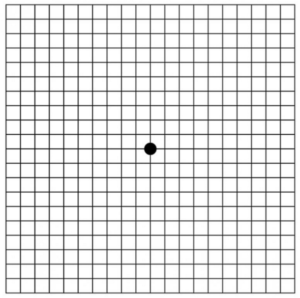
- Amsler Grid: Regularly monitor your vision at home using an Amsler grid. Notify your eye doctor immediately if you notice any new blind spots, distortions, or other changes on the grid.
- Diet: Include antioxidants from fruits and green vegetables in your diet, as they have been shown to reduce the risk of AMD. Additionally, frequent consumption of fish high in omega-3 fatty acids is beneficial.
- Smoking: Quitting smoking is strongly recommended, as it has been linked to an increased risk of AMD.
- Sun Protection: Protect your eyes from sun damage, which has been associated with AMD.
For those who have already experienced vision loss due to AMD, numerous resources are available. Support groups and psychological counseling can aid in adjusting to life with reduced vision. Low-vision specialists offer valuable assistance, helping patients use their peripheral vision effectively and recommending magnification devices and daily living aids. Many patients discover that with the right tools and training, daily tasks can be accomplished independently, allowing for a surprisingly normal and fulfilling life.
Where Can I Get More Information?
At Milwaukee Eye Care, our priority is to provide you with compassionate care while staying at the forefront of advancements in ophthalmology. To schedule an appointment with Dr. Mackenzie Sward, please call 414-271-2020 or schedule online.