Keratoconus is a disease of the cornea, which is the normally clear, front surface of the eye and the part of the eye on which contact lenses are worn. If the clear front surface of the eye is damaged, cloudy, or has an irregular surface, perfectly clear vision is not possible. This is similar to a camera lens, which if scratched or cracked, will not allow the camera to take high quality pictures. In keratoconus, the cornea develops an abnormal thinning and irregular shape, causing distortion of light rays passing through it. This results in blurred vision that cannot be corrected with eyeglasses.
The exact cause of keratoconus is unknown, although research points strongly to a genetic predisposition. The diagnosis is initially made during an eye exam, when an irregular corneal curvature makes it impossible to correct vision to normal levels using eyeglass lenses. Detailed mapping of the entire corneal curvature, known as topography, is a test that’s helpful in making the diagnosis. Sometimes, the corneal curvature is only mildly abnormal. This is often referred to as “forme fruste” keratoconus, which means a mild or incomplete form of the disease.
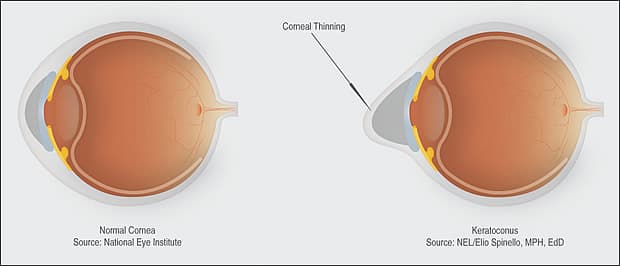
Keratoconous usually starts when patients are adolescents or young adults and continues into their 30s, at which point progression of the disease either slows or stops. Males and females are equally affected. Signs of keratoconus are usually present in both eyes, although one eye may have much more involvement than the other. When patients are young, the condition can be progressive, leading to an irregular outward protrusion of the cornea, known as ectasia. In advanced disease, this protrusion causes the cornea to develop a steepened “cone” shape when looked at from the side, which is why the disease was given the name keratoconus. Middle aged patients with keratoconus, whose vision can be clearly corrected with contact lenses, are unlikely to ever develop more severe disease. Patients with advanced keratoconus can experience sudden episodes of painful corneal swelling, known as hydrops, that can lead to opacification and scarring of the cornea, with permanent vision loss.
Treatment
The treatment of keratoconus depends on how severe it is. For early or mild cases, eyeglasses may correct vision to levels that are sufficient for most normal activities, even though those patients may not see 20/20. When vision can no longer be adequately corrected with glasses, soft contact lenses, either spherical or more commonly “toric” contact lenses that correct astigmatism, are used. There are many specialized types of contact lenses to help people with keratoconus. Some of these lenses even combine soft and rigid lens materials. The vast majority of patients with keratoconus depend on rigid gas permeable contact lenses to achieve vision that is good enough to carry out normal daily activities. When contact lenses can no longer provide adequate vision correction, surgical treatment is the next step.
On a worldwide basis, keratoconus is one of the leading reasons for corneal transplant surgery, becoming necessary in 10-20% of those with the disease. There are a number of other promising new treatments aimed at preventing progression of the disease. Some of these procedures are variations of corneal transplant surgery that involve replacing partial layers of the cornea, sometimes utilizing lasers. For patients that are young and show rapid progression, collagen cross-linking has shown promise. This is a procedure that “freezes” and stabilizes the shape of the cornea. When patients develop extensive disease, they may be eligible for intracorneal rings, the most common of which is called INTACS. These devices are surgically inserted in the cornea, flattening it, and allowing some patients to achieve better vision with contact lenses. INTACS may also be combined with collagen cross-linking.
Keratoconus is a condition that can lead to varying levels of visual disability, but there are many treatment options available. Deciding on the best treatment for you depends on an evaluation by your eye doctor and a discussion of your visual needs.
To schedule an appointment for a corneal evaluation with Dr. Edmonds, please call Milwaukee Eye Care at 414-271-2020.